AI in pediatric brain cancer prediction marks a significant advancement in the fight against childhood cancer, specifically targeting the challenging arena of gliomas. Recent studies have shown that this innovative technology can outperform traditional methods in predicting tumor relapse, offering new hope for pediatric patients. By analyzing a series of brain scans over time using AI medical imaging, researchers can identify subtle changes that signal a risk of recurrence, which is crucial for timely intervention. The incorporation of temporal learning in oncology enhances the accuracy of predictions, thus potentially transforming treatment pathways and alleviating the burden on families. As advancements in childhood cancer treatment continue, the focus on AI-driven solutions underscores the importance of harnessing technology for better patient outcomes and improved quality of life for young survivors.
The application of artificial intelligence in predicting pediatric brain cancer recurrence represents a groundbreaking development in the medical field, particularly concerning childhood gliomas. By leveraging advanced imaging techniques and longitudinal data analysis, researchers are uncovering vital patterns that traditional assessments often overlook. This shift towards a more predictive model could revolutionize how doctors monitor and treat young patients battling brain tumors. The integration of temporal learning approaches allows for a comprehensive understanding of tumor behavior over time, enabling more personalized treatment strategies. As the conversation around childhood cancer treatment advancements evolves, the role of AI becomes increasingly prominent, offering newfound optimism for families facing these daunting challenges.
Understanding Pediatric Brain Cancer: Gliomas and Their Challenges
Pediatric brain cancer, particularly gliomas, represents one of the most challenging domains in childhood oncology. These brain tumors can have varying levels of aggressiveness and complicated treatment paths. While many gliomas are treatable, relapses pose a significant risk, necessitating ongoing vigilance. The complexity of treatment decisions and patient management can be daunting for families and healthcare providers alike.
Factors influencing the risk of recurrence in pediatric gliomas include tumor type, location, and grade. Understanding these variables plays a critical role in developing effective treatment plans. Advances in medical imaging and predictive analytics are crucial in helping clinicians navigate the uncertainties surrounding glioma treatment. Early identification of patients at high risk for relapse can greatly improve clinical outcomes and reduce the emotional and financial burden on families.
AI in Pediatric Brain Cancer Prediction: A Game Changer
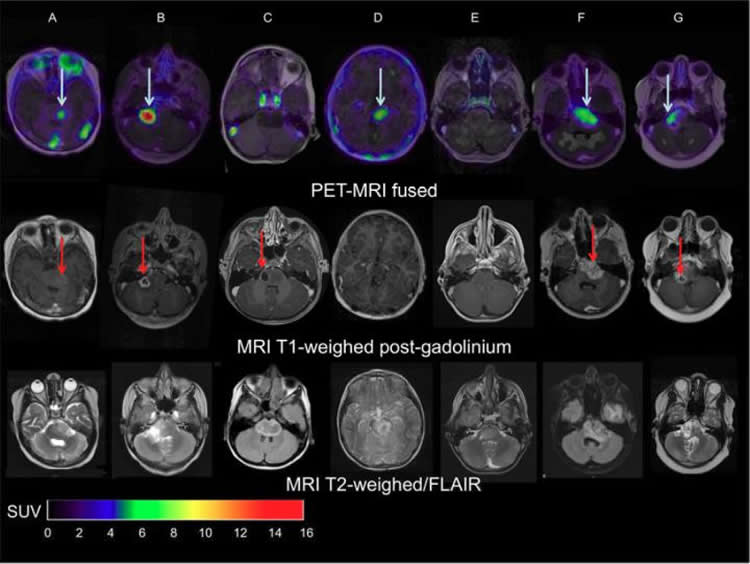
Artificial Intelligence (AI) is transforming the landscape of pediatric brain cancer prediction and management, particularly in the realm of glioma relapse prediction. Recent studies, including those from prestigious institutions like Harvard, have shown that AI tools outperform traditional methods in assessing the risk of cancer recurrence. By analyzing repeated MR scans, the AI system can detect subtle changes that may indicate a shift in a patient’s condition.
The use of AI in pediatric brain cancer predictions exemplifies how technology can elevate conventional medical practices. Moreover, with techniques such as temporal learning, these AI systems learn over time from sequential imaging data, which significantly enhances the accuracy of relapse predictions. This innovative approach positions AI as an indispensable ally in developing personalized treatment pathways for children facing brain tumors.
The Role of Temporal Learning in Oncology
Temporal learning is an exciting, emerging technique in the field of oncology that allows AI models to learn from serial imaging data. Unlike traditional models that rely on single snapshots, temporal learning leverages the dynamic progression of a patient’s condition observed through multiple MRI scans. This method is particularly beneficial for predicting the likelihood of glioma recurrence, as it incorporates a broader context of the disease progression.
By training models to recognize patterns and changes within a timeline of stored images, researchers have enhanced the predictive capabilities of AI regarding pediatric brain cancer recurrences. Early results suggest that combining historical data with advanced imaging techniques enriches the dataset, thereby improving predictive accuracy, which is invaluable for formulating proactive treatment strategies.
Childhood Cancer Treatment Advancements
Advancements in childhood cancer treatment over the past few decades have paved the way for improved survival rates and quality of life for pediatric patients. Innovative therapies, including targeted treatments and immunotherapy, are being increasingly integrated into clinical practice to tackle the complexities of pediatric cancers, particularly gliomas.
Moreover, the inclusion of AI technologies in treatment protocols signals a significant shift towards precision medicine. Treatments tailored to individual patient profiles and tumor characteristics are crucial for optimal outcomes. With ongoing research and clinical trials, including the exploration of AI in glioma management, the future looks promising for effective interventions in childhood brain cancer.
The Importance of Continuous Monitoring in Pediatric Gliomas
Patients recovering from gliomas face a landscape of continuous monitoring to catch potential relapses early. This constant vigilance helps healthcare providers implement interventions promptly should a recurrence occur. Traditional follow-up methods often rely on regular imaging, which can be emotionally taxing for young patients and their families.
Incorporating AI into the monitoring process allows for a more streamlined and less invasive approach. By facilitating intelligent predictions based on comprehensive imaging data, clinicians can adjust follow-up frequencies and only subject patients to necessary scans. This strategic approach not only alleviates patient burden but also fosters better public health outcomes by ensuring timely interventions.
AI Medical Imaging: Revolutionizing Pediatric Oncology
AI medical imaging is at the forefront of transforming pediatric oncology, particularly in the early detection and management of brain tumors. By employing sophisticated algorithms to analyze imaging studies, AI can identify patterns and risks that human eyes might overlook, aiding in more informed clinical decisions. This shift toward AI-assisted diagnostics can lead to earlier interventions and better prognoses for pediatric patients.
The ability of AI to assess vast amounts of imaging data rapidly supports clinical professionals in their ongoing efforts to provide effective and timely care. Furthermore, as AI technologies evolve, their integration with other treatment modalities presents exciting opportunities for enhanced patient management and outcomes in childhood cancers, especially those as complex as gliomas.
The Future of Pediatric Brain Cancer Care
The future of pediatric brain cancer care is poised for a remarkable transformation, driven by the integration of AI technologies and advanced medical imaging techniques. As researchers and clinicians continue to explore the potential of AI in predicting glioma relapses, the landscape of treatment protocols will likely evolve significantly. Innovations such as temporal learning will empower professionals to craft more effective, individualized treatment strategies.
In this evolving paradigm, continuous research and clinical trials will be essential to validate the efficacy of AI predictions in real-world settings. Ultimately, these advancements aim to enhance treatment outcomes, reduce distress during follow-up care, and foster a supportive environment for pediatric patients and their families navigating the challenges of childhood cancers.
Collaboration in Pediatric Brain Cancer Research
Collaboration among institutions is a key component in advancing pediatric brain cancer research, particularly in developing innovative AI strategies for glioma management. Partnerships between leading hospitals, research universities, and cancer care networks foster the exchange of knowledge, resources, and innovative practices that can significantly enhance treatment pathways for children.
By pooling data from multiple sources, researchers can develop more comprehensive AI models that are better equipped to predict relapse risks. Collaborative efforts also help attract funding and support for vital studies that further the understanding of pediatric brain tumors and the implementation of cutting-edge treatment methodologies.
Patient-Centric Approaches in Managing Pediatric Brain Cancer
A patient-centric approach is essential in managing pediatric brain cancer, ensuring that treatment strategies align with the unique needs and experiences of young patients and their families. Incorporating AI technologies helps personalize treatment plans and monitor patient progress in a way that respects their emotional and physical well-being. This integrated care model focuses not only on clinical outcomes but also on the patient’s quality of life.
Establishing open communication channels between healthcare professionals, patients, and families is integral to effective management of pediatric brain cancer. As advancements in AI and imaging foster proactive treatment options, the emphasis remains on providing holistic and compassionate care within the context of emerging technologies.
The Role of Feedback in AI Development for Oncology
Feedback mechanisms are crucial in the iterative process of developing AI tools for oncology, particularly regarding pediatric brain cancer management. Continuous feedback from clinicians who utilize AI predictions can significantly enhance the model’s accuracy and effectiveness. This collaboration ensures that AI systems evolve in line with clinical realities, addressing real-world challenges faced by healthcare providers.
Implementing robust feedback systems allows for the refinement of algorithms based on diverse clinical experiences and outcomes. As AI becomes more entrenched in pediatric oncology, establishing effective channels for feedback will be paramount in ensuring these tools contribute meaningfully to patient care and treatment success.
Frequently Asked Questions
What role does AI play in pediatric brain cancer prediction?
AI enhances pediatric brain cancer prediction by analyzing multiple MRI scans over time, allowing for more accurate predictions of glioma relapse risk compared to conventional methods. This usage of AI medical imaging techniques enables healthcare providers to identify at-risk patients earlier, improving treatment decisions.
How does temporal learning improve AI in pediatric brain cancer prediction?
Temporal learning improves AI in pediatric brain cancer prediction by allowing the model to synthesize information from multiple consecutive MRI scans. This method enhances the accuracy of predicting glioma relapse by recognizing subtle changes that occur over time, leading to prediction improvements of 75-89%.
Why is AI important for predicting glioma relapse in children?
AI is crucial for predicting glioma relapse in children as it offers a more precise risk assessment than traditional imaging methods. By utilizing advanced AI medical imaging techniques, clinicians can better identify patients needing intensive follow-up and treatment, potentially reducing stressful repeat imaging for lower-risk individuals.
What advancements are being made in childhood cancer treatment through AI?
Advancements in childhood cancer treatment through AI include improved predictive analytics for gliomas and other pediatric brain cancers. AI tools facilitate better understanding and prediction of cancer recurrence, leading to personalized treatment plans that can reduce unnecessary procedures and focus on targeted therapies for high-risk cases.
How does AI compare to traditional methods in predicting pediatric brain cancer outcomes?
Studies show that AI significantly outperforms traditional methods in predicting pediatric brain cancer outcomes, particularly glioma relapse. The use of AI medical imaging enables more nuanced predictions drawn from temporal learning, providing healthcare professionals with reliable data to enhance patient care and treatment strategies.
What is the significance of the recent study on AI in pediatric brain cancer prediction?
The recent study highlights the effectiveness of an AI model in predicting glioma relapse with higher accuracy than traditional imaging methods. This research advances the field of pediatric oncology by demonstrating how AI can analyze longitudinal imaging data, enhancing early intervention strategies and overall patient management.
Can AI reduce the burden of follow-up imaging for pediatric glioma patients?
Yes, AI has the potential to reduce the burden of follow-up imaging for pediatric glioma patients by accurately identifying low-risk individuals who may not require frequent scans. By improving glioma relapse predictions, AI enables more tailored follow-up care that alleviates stress for children and families.
What future directions are expected for AI in pediatric oncology?
Future directions for AI in pediatric oncology include further validation of AI-driven predictive models and the launch of clinical trials. These initiatives aim to explore the clinical implications of AI-informed risk predictions, potentially transforming protocols for managing pediatric brain cancer treatments.
| Key Points | Details |
|---|---|
| AI Tool Accuracy | Outperforms traditional methods in predicting relapse risk for pediatric glioma patients. |
| Study Publication | Published in The New England Journal of Medicine AI with research conducted by Mass General Brigham and collaborators. |
| Temporal Learning Technique | Uses multiple brain scans over time to improve prediction accuracy, rather than relying on single images. |
| Prediction Accuracy | Achieved 75-89% accuracy for predicting recurrence, compared to approximately 50% for single image analysis. |
| Clinical Implications | Could help reduce imaging frequency for low-risk patients and guide treatment for high-risk patients. |
Summary
AI in pediatric brain cancer prediction is revolutionizing how healthcare providers approach the treatment and monitoring of children with brain tumors such as gliomas. By employing advanced machine learning techniques, including temporal learning, researchers are now able to predict relapse risks with remarkable accuracy, significantly enhancing patient care outcomes. As this study demonstrates, the transition from traditional methods to AI-driven tools can alleviate the burden on pediatric patients and their families, while also paving the way for targeted therapies in high-risk cases. The growing body of evidence surrounding AI applications in oncology underscores the potential for these technologies to reshape medical practices and improve prognostic capabilities.