TIM-3 therapy for Alzheimer’s disease represents a groundbreaking approach in the fight against this debilitating condition. Recent research indicates that leveraging TIM-3, an inhibitory checkpoint molecule usually employed in cancer treatment, may transform Alzheimer’s treatment as we know it. By inhibiting TIM-3, scientists have observed promising results in mice, where microglia—brain immune cells—are empowered to clear amyloid plaques and enhance memory function. This revolutionary strategy addresses not only the accumulation of toxic plaques but also highlights the intricate relationship between the immune system and Alzheimer’s pathology. Such innovations could redefine how we tackle Alzheimer’s, moving closer to a solution that restores cognitive function and improves patients’ quality of life.
In the realm of Alzheimer’s therapy, TIM-3 is emerging as a pivotal molecule that could alter the course of treatment for many affected individuals. This therapy harnesses the potential of immunological checkpoints to revitalize the brain’s immune response, effectively enabling microglia to clear out harmful plaques associated with dementia. The implications of this approach are far-reaching, as it bridges the concepts of cancer immunotherapy with neurodegenerative disease management. As researchers delve deeper into this field, understanding the interplay of the immune system and Alzheimer’s becomes increasingly vital. Ultimately, advancements in TIM-3 targeting strategies may pave the way for innovative therapeutic avenues in combating memory loss and cognitive decline.
Understanding TIM-3 Therapy for Alzheimer’s Disease
TIM-3, or T-cell immunoglobulin and mucin-domain containing-3, is a checkpoint molecule that plays a critical role in regulating the immune system. In the context of Alzheimer’s disease, TIM-3 restricts the activity of microglia, the brain’s immune cells, preventing them from effectively clearing amyloid plaques that contribute to cognitive decline. Recent research has indicated that by inhibiting TIM-3, we can unleash the potential of microglia to target these plaques, potentially restoring cognitive function in affected individuals.
The implications of TIM-3 therapy could be profound, as it represents an innovative approach to treating Alzheimer’s disease. Traditional Alzheimer’s treatments have focused primarily on combating the amyloid beta plaques themselves, but by utilizing a strategy that adjusts the immune response, TIM-3 therapy offers a new pathway for therapeutic intervention. This is particularly relevant given the genetic link between TIM-3 polymorphisms and the risk of developing late-onset Alzheimer’s, making it a promising target for personalized medicine in neurodegenerative diseases.
The Role of Microglia in Alzheimer’s Progression
Microglia are the brain’s resident immune cells, responsible for maintaining homeostasis and modulating inflammation. In Alzheimer’s disease, these cells often become dysfunctional, leading to an inability to clear amyloid plaques and resulting in further neurodegeneration. The activation of microglia typically prompts an increase in the expression of inhibitory molecules like TIM-3, which effectively puts them in a dormant state. This halt in action allows for the accumulation of harmful substances in the brain, exacerbating cognitive decline.
Research has shown that the deletion of TIM-3 in microglia can enhance plaque clearance and restore cognitive function in mouse models of Alzheimer’s. By stimulating microglial activity through TIM-3 inhibition, researchers have noted significant improvements in memory and cognitive behaviors, suggesting that targeting microglia may be an essential component in the fight against Alzheimer’s disease. As studies continue to explore this potential, understanding the complex functions of microglia remains crucial.
Checkpoint Molecules: A Key Connection in Alzheimer’s Disease
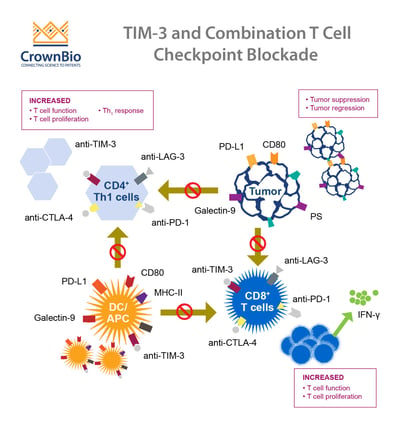
Checkpoint molecules, like TIM-3, are essential for preventing overactivation of the immune system. These molecules act as safeguards, ensuring that once the body has responded to an infection or injury, immune activity is scaled back to avoid harm to healthy tissues. In the context of Alzheimer’s, the role of checkpoint molecules becomes more complicated, as their overexpression can lead to microglial inactivity at a time when they are needed most to clear harmful plaques.
The challenge lies in finding ways to modulate these checkpoint pathways effectively. While current cancer treatments exploit these molecules to enhance anti-tumor immunity, the same principles can be applied to neurodegenerative diseases like Alzheimer’s. By understanding how to manipulate TIM-3 and similar molecules, researchers hope to develop therapies that not only improve immune responses in the brain but also enhance overall treatment outcomes for Alzheimer’s patients.
Crossover Between Cancer Treatment and Alzheimer’s Disease
Interestingly, the strategies employed in cancer immunotherapy may also have implications for treating Alzheimer’s disease. Both conditions involve the immune system’s mechanisms; in cancer, checkpoint inhibitors enhance immune responses against tumor cells, while in Alzheimer’s, the inhibition of TIM-3 may reactivate microglia to combat plaque buildup. This crossover suggests a shared pathway that could lead to innovative therapeutic approaches that address both cancer and neurodegeneration.
Utilizing existing anti-TIM-3 antibodies, initially developed for cancer treatment, could facilitate rapid advancements toward effective Alzheimer’s therapies. The success seen in some cancer patients lays a promising groundwork. The potential to repurpose these treatments for Alzheimer’s disease not only saves time and resources but also paves the way for future developments that could significantly improve patient outcomes.
Advancements in Alzheimer’s Treatment Strategies
Developing effective treatment for Alzheimer’s has been a significant challenge, highlighted by several high-profile drug trial setbacks. However, recent advancements herald a new era in treatment strategies. The focus on immune checkpoint inhibition, particularly TIM-3, signifies a paradigm shift in how we approach Alzheimer’s therapy. By enhancing the brain’s immune response, we may tackle the underlying mechanisms of the disease more effectively than by simply targeting the symptoms.
Research in this area is quickly evolving, with studies showing that modifying TIM-3 expression can lead to tangible improvements in cognitive behavior in preclinical models. This refreshing approach suggests that future therapies might center on immunomodulation, which could lead to new drugs designed to enhance the brain’s natural ability to clear amyloid plaques and improve memory function.
The Future of TIM-3 Inhibitory Therapies
Looking ahead, TIM-3 inhibitory therapies could revolutionize the landscape of Alzheimer’s treatment. As research continues, the aim is to translate findings from animal models to human applications effectively. The focus will likely shift from merely alleviating symptoms to addressing the root causes of the disease by restoring normal microglial function and thereby improving cognitive health.
Moreover, with the integration of genetic studies that identify TIM-3 as a risk factor for late-onset Alzheimer’s, there is potential for personalized medicine approaches that tailor treatments to individual genetic profiles. This could make TIM-3 therapies not only innovative but also specifically effective for those most at risk for developing Alzheimer’s.
Connection Between Inflammation and Alzheimer’s Disease
Recent studies have indicated a strong connection between chronic inflammation and the onset of Alzheimer’s disease. The brain’s immune response, mediated by microglia, plays a crucial role. When inflammation persists, it can lead to an exacerbation of neurodegenerative processes, harming neuronal health and function. The expression of receptors like TIM-3 may contribute to this cycle by silencing microglial activity when it is most needed, illustrating a critical intersection between immune function and cognitive decline.
Addressing inflammation through TIM-3 modulation could bring a twofold benefit: rejuvenating microglial activity to clear out amyloid plaques while also potentially mitigating the inflammatory damage that accelerates Alzheimer’s progression. This highlights the importance of investigating the inflammatory pathways and how interventions can modify them to protect neuronal function.
Significance of Genetic Factors in Alzheimer’s Disease
The role of genetic factors in Alzheimer’s disease risk has significantly advanced our understanding of the disease. Identifying specific polymorphisms in genes like TIM-3, which correlate with increased Alzheimer’s risk, emphasizes the importance of genetic research in crafting targeted therapies. Such insights enable researchers to focus on individuals who might benefit most from TIM-3 inhibition as a potential therapy, enhancing the precision of treatment approaches.
Understanding genetic predispositions also allows for earlier interventions. If individuals with certain TIM-3 polymorphisms can be identified early, proactive therapeutic strategies can be employed. This genetic perspective complements traditional approaches by incorporating personalized strategies that hold promise for altering the disease trajectory in high-risk populations.
The Impact of Alzheimer’s on Public Health
Alzheimer’s disease is increasingly recognized as a growing public health crisis, affecting millions globally. As the population ages, the incidence of this debilitating condition is projected to rise significantly. The urgency for effective treatments is further compounded by the immense healthcare costs associated with managing Alzheimer’s, emphasizing the need for innovative strategies like TIM-3 therapy, which could reshape how we approach care, prevention, and treatment.
The broad implications of breakthrough therapies extend beyond individual patients; they could alleviate the strain on healthcare systems and improve quality of life for countless families. Hence, advancing research into therapies like TIM-3 not only holds potential for treating Alzheimer’s disease effectively but also promises to have a profound societal impact.
Frequently Asked Questions
What is TIM-3 therapy for Alzheimer’s disease?
TIM-3 therapy for Alzheimer’s disease refers to the use of anti-TIM-3 antibodies or small molecules that block the TIM-3 inhibitory pathway, enhancing the ability of microglia, the brain’s immune cells, to clear amyloid plaques associated with Alzheimer’s. This therapy aims to improve cognitive function by promoting plaque clearance.
How does TIM-3 affect microglia function in Alzheimer’s disease?
In Alzheimer’s disease, TIM-3 inhibits microglia from engulfing toxic amyloid plaques, leading to plaque accumulation in the brain. By blocking TIM-3, researchers aim to unleash microglial activity, allowing these immune cells to clear plaques and improve brain health and cognitive performance.
What are the potential benefits of TIM-3 therapy compared to traditional Alzheimer’s treatments?
TIM-3 therapy for Alzheimer’s disease offers a novel approach compared to traditional treatments by targeting immune checkpoint mechanisms, potentially leading to better plaque clearance. Unlike conventional therapies, which have had mixed success, TIM-3 therapy shows promise in enhancing microglial function and improving cognitive outcomes in studies.
What role does the TIM-3 molecule play in Alzheimer’s treatment?
The TIM-3 molecule functions as an immune checkpoint in the brain, inhibiting microglia from clearing Alzheimer’s-related amyloid plaques. By targeting TIM-3 with specific therapies, researchers aim to restore the natural immune response in the brain, enhance plaque clearance, and ultimately improve memory and cognition in Alzheimer’s patients.
Can TIM-3 therapy for Alzheimer’s disease also be used in cancer treatment?
Yes, the TIM-3 pathway has been studied extensively in cancer treatment, where TIM-3 is targeted to enhance anti-tumor immunity. The strategy being researched for Alzheimer’s disease explores the dual role of TIM-3 as a checkpoint molecule, suggesting that therapies designed for cancer may also be effective in treating Alzheimer’s.
What findings were observed in mice treated with TIM-3 therapy for Alzheimer’s disease?
Mice genetically modified to lack the TIM-3 gene showed improved plaque clearance and cognitive function in Alzheimer’s disease models. These studies demonstrated that blocking TIM-3 enables microglia to more effectively clear amyloid plaques, leading to significant improvements in memory performance and behavior.
How long will it take to develop TIM-3 therapy for human Alzheimer’s patients?
While initial studies have shown promising results in animal models, translating TIM-3 therapy for human use requires extensive further research, including clinical trials to ensure safety and efficacy. This process may take several years, with ongoing studies to test human anti-TIM-3 in Alzheimer’s mouse models.
What specific challenges exist when developing TIM-3 therapies for Alzheimer’s?
Developing TIM-3 therapy for Alzheimer’s faces challenges such as ensuring the therapy effectively crosses the blood-brain barrier and minimizing potential side effects. Additionally, the complexity of Alzheimer’s pathology and the variability in patient response must be considered during the therapeutic development process.
| Key Point | Details |
|---|---|
| Potential of TIM-3 Therapy for Alzheimer’s Disease | Research indicates that blocking TIM-3 can allow microglia to clear Alzheimer’s plaques, improving memory and cognition in mice. |
| Role of TIM-3 in Immune Regulation | TIM-3 acts as a checkpoint molecule that inhibits microglia from attacking amyloid plaques due to increased expression in Alzheimer’s. |
| Link to Late-Onset Alzheimer’s | The TIM-3 molecule is genetically associated with late-onset Alzheimer’s, which constitutes 90-95% of cases. |
| Impact on Microglia Functionality | Deletion of the TIM-3 gene enhances microglial activity, allowing them to effectively clear plaques. |
| Future Research Directions | Next steps involve testing human anti-TIM-3 antibodies to determine efficacy in halting plaque development in Alzheimer’s models. |
Summary
TIM-3 therapy for Alzheimer’s disease is a promising approach based on groundbreaking research that reveals the potential of an immune-system strategy derived from cancer treatments. By blocking the TIM-3 checkpoint molecule, researchers have observed a significant restoration of cognitive function in mouse models of Alzheimer’s. This innovative therapy could not only enhance memory by allowing microglia to clear harmful plaques but also offer new hope following previous drug trial failures. As studies progress towards human applications, TIM-3 therapy offers a unique and targeted avenue for treating Alzheimer’s disease.